Erasmus+
“This project has been funded with support from the European Commission. This publication reflects the views only of the author, and the Commission cannot be held responsible for any use which may be made of the information contained therein”
Counseling techniques applied during the rehabilitation period
Upon completion of this module the reader will be able to:
- Understand the importance of incorporating counselling and communication skills between the exercise expert and the injured athletes
- Understand basic counselling skills between the exercise expert and the athletes that enhance injured athletes’ motivation
- Understand the emotional status of the injured athlete and its needs
- Determine appropriate counselling techniques for specific components of the rehabilitation plan
- Incorporate a mental training program into the training sessions of the injured athletes
First, it is strongly suggested to review Module 1 referring to the “Counseling techniques applied during the rehabilitation period”.
One of the great dangers an athlete can face, if not the greatest, is the risk of getting injured. That’s why its prevention and treatment constitute an essential part of the medical and performance department of the clubs. However, a part not yet explored about this risk has to do with the athlete’s psychological and social factors.
According to Andreas Ivarsson, PhD in psychology at the University of Halmstad, in Sweden, and Head of Psychology and personal development at Arsenal F.C., there are a few main mechanisms for the relationship between stress and injury risk. One of these is that stress will negatively influence the athlete’s abilities to take high qualitative decisions due to a narrowed peripheral vision. Another proposed mechanism is that stress is likely to generate higher levels of psychophysiological fatigue. An increase in fatigue might, in turn, increase the risk of becoming injured.
Read carefully the description of these techniques as they can also be used by healthy athletes for injury prevention.
Ivarsson, A., Johnson, U., Karlsson, J., Börjesson, M., Hägglund, M., Andersen, M. B., …Waldén, M. (2018). Elite female footballers’ stories of sociocultural factors, emotions, and behaviors prior to anterior cruciate ligament injury. International Journal of Sport and Exercise Psychology. Advance online publication.
Counseling techniques applied during the rehabilitation period
When athletes sustain injuries, the primary focus of sports medicine professionals is, understandably, on the physical aspects of treatment and recovery. But, in addition to the physical consequences of sport injury, the psychological functioning of athletes may also be profoundly affected by injury. This means that, injury may have a significant impact on the emotional status of athletes [10]. Sports medicine professionals have also reported that injured athletes are often in need of certain psychological interventions to overcome the emotions and behaviours experienced after their injury [4, 36, and 65]. If understood and used properly, these strategies can be important tools for effective rehabilitation. Additionally, for many people physical injury and its treatment and rehabilitation can be extremely stressful. For athletes who obtain self-esteem, personal motivation and competence from their performances, injury and its accessories, can be emotionally devastating. These strategies can help and improve the rehabilitation process and also “push” the athletes re-establish their athletic identity.
Wondering who can use these tools effectively, it is evident that sports medicine professionals are often the most influential people in the lives of injured athletes as they attempt to recover from their injuries [36]. When injured athletes respect and truly trust their therapist, they build their confidence during all the rehabilitation period and they have a slow but steady return to their competitive performances. Physical therapists and athletic trainers have a particular advantage in establishing psychological care relationships. This particular advantage relates to the power of “touch”, meaning the physical contact that is necessary between the therapist and the athlete. This is not only an integral and accepted part of physical therapy treatment. It is also a powerful tool of communication [43]. Some people may feel inhibited by the “touch” of physical therapies, but the majority free up their emotions and relax [47]. Therefore, athletes may open up more to physical therapists and athletic trainers than to some other medicine professionals.
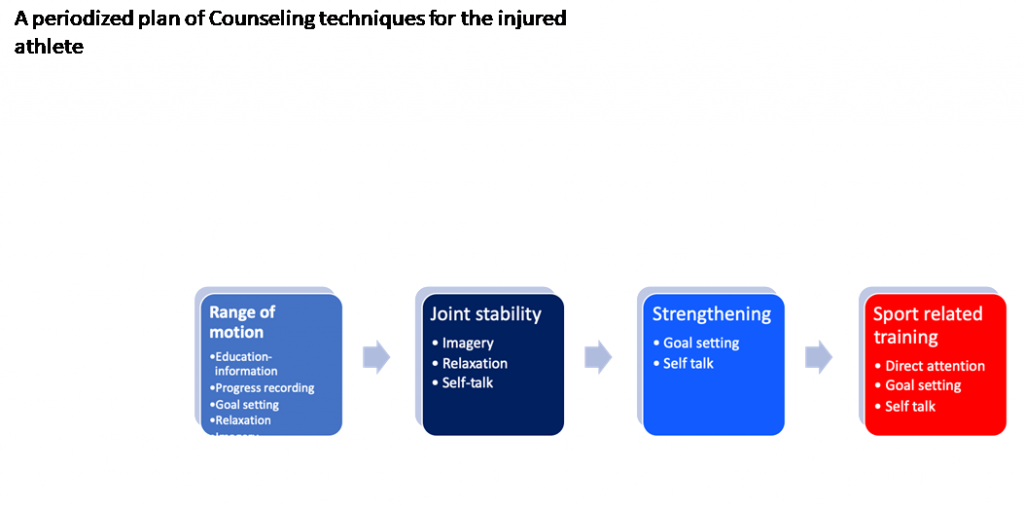
Thus, providing those specialists with a “periodized” plan may make it easier for them to both identify and implement mental skills-training technique in conjunction with the physical rehabilitation plan [15]. The goal of the present study is to propose counselling techniques that could be applied also by physical therapists and athletic trainers during specific components of the rehabilitation period, helping their athletes cope with pain and negative feelings, and keep their motivation to the rehabilitation program. It is not within the scope of this article to present in detail each counselling technique. The authors aim to suggest how to incorporate these techniques in specific rehabilitation components.
Emotional situation of the injured athlete and counselling techniques
It is reported that some athletes experiencing extreme depression after sustaining an injury have gone so far as to attempt suicide [58]. Across several studies, injured athletes have consistently described the early period of rehabilitation as marked by feelings of anger, confusion, depression, fear and frustration [7, 27, 33, 60, and 67]. Athletes have also reported that as rehabilitation progresses, the negative emotions emanating most frequently from injury-related disruption of functioning tend to be depression and frustration. Reports of depression and frustration have been common even as rehabilitation nears completion and a return to sport is imminent [10]. Furthermore, athletes have cited the fear of re-injury as a salient emotion associated with resuming sport participation [7, 33].
This is the reason why sport physiotherapists and sport/athletic trainers believe that many counselling techniques should be part of their professional education [36]. In more specific, they believe that the following skills are important and desirable components of their education: Collaborative goal setting; [65] motivation techniques; imagery; positive self-talk [4]; effective communication skills and counselling; arousal control and anxiety management; confidence and assertiveness training; concentration and attention; cognitive restructuring; reduction of depression; pain management; relaxation and the provision of social support [9, 12, 23, 27, 32, 37, 38, 39, and 69]. Furthermore, it is believed that these techniques could improve the interaction between the injured athlete and sports medicine personnel [3, 13, 19, 29, 53, and 55]. These techniques can be applied during rehabilitation to help athletes cope with pain and anxiety [63], deal with negative and irrational thinking, and assist with motivation and compliance [62, 65].
Appropriate counselling techniques for specific components of the rehabilitation plan
Obtaining normal range of motion – Coping with pain
The primary emphasis in the rehabilitation plan is usually given on improving the range of motion of the injured area [61]. In order to obtain the normal range of motion again, the injured area has to be stressed. But, this is very painful procedure for athletes that require also complex techniques from the therapist such as manual therapy. Consequently, the first challenge that athletes have to deal with is pain [50]. Pain is so significant at this early stage because it is always inevitable, usually severe, sometimes unknown, and typically outside the control of the athletes [54]. However, pain is a component of many injury rehabilitation programs, and this fact is problematic for rehabilitation adherence. Although for most people in most situations, pain is a signal to stop the activity that is causing the pain, injured athletes on the other hand, need to work through particular aspects of their pain sensations for maximizing their rehabilitation efforts [51].
Can anything be done about how injured athletes react to this potentially painful procedure? Pain has both physiological and psychological properties; it hurts, but the magnitude of the sensation depends on the injured athletes’ perception and labelling [51]. Pain tolerance depends on their capacities to handle pain and the importance they place on their rehabilitation. Athletes who believe in the efficacy of their treatment programs and believe in their ability to adhere to these programs are better able to cope with their pain. These positive beliefs and attitudes lead to increased resourcefulness and persistence in applying coping strategies, enhanced mobilization of cognitive resources to direct attention away from pain sensation, and even reduced distressing anticipation of pain [71]. At the very least, sports medicine professionals should assist injured athletes in understanding the nature of pain they might encounter.
Education about this pain
The first thing the therapist is recommended to do is to educate them about what to expect, especially as they start to become more mobile. In other words, therapists need to describe the feeling that athletes are likely to experience while doing the necessary range of motion exercises. Expressions such as, “don’t be surprised if you feel a little tenderness on the inside of your knee” can prepare athletes for what they expect. So pain description is the first tool, but it is not enough.
As the rehabilitation progresses, the therapist has to assist athletes distinguish between that pain associated with healing and that pain which may signal further injury: “You might feel some tightness in the inside of your knee as you rotate it, but that’s good because you need to stretch it out”. The distinction between “good pain” and “bad pain” is getting more important as uncertainty leads to more anxiety and increased anxiety might predispose athletes to reduced commitment [24]. With more information and knowledge comes reduced uncertainty, which leads to a greater sense of commitment and more effort for recovery [45].
Progress recording and goal setting
Another way to help athletes deal with pain and tolerate it, is to record their progress. It is crucial for athletes to realize the incremental improvement made. Second, they should be reminded that every trial of each exercise gets them closer to recovery [24].
As long as athletes see their improvement they can set a goal about their next trial. In recent years a number of training strategies have been identified as ways of assisting athletes in different phases through their personal growth and development. Additionally, in rehabilitation, goal setting plays an important role. In fact, goal setting has not only showed its influence on the athletes’ performance, but has also been linked to positive changes in major psychological states such as anxiety, confidence, motivation and coping with injury. Locke, Shaw, Saari, and Latham [42] defined as goal “attaining a specific standard of proficiency on task, usually within a specified time limit” (p. 145).
While athletes are in pain it would be very beneficial to direct their attention to “gain more degrees”. For example, at this moment the therapist measures the range of motion and informs the athlete that he has already gained 45 degrees of dorsi flexion. The athlete thinks, “I have my ankle flexed at 45degrees. I will try again to obtain a flexion of 50 degrees” and so he tries again. It is well documented that this specific, difficult, and challenging goal can enhance the athlete’s effort more than easy goals, no goals, or vague goals like “do your best” [15].
In conclusion, pain description and distinction; improvement recording and goal setting can help athletes “come through” their pain.
Relaxation
While working for normal range of motion, many athletes have the fear of re-injury as the physical therapist may stretch the injured area in a way that reminds the athletes of how they have got injured. Athletes are usually worried about re-injury and because of this they are likely not to be relaxed. As a result, muscular tension -caused by anxiety- increases sensations of pain [57].
To face that problem, athletes should apply a relaxation technique, focusing particularly on muscles involved. Using the relaxation technique athletes really can see and feel definite gains in flexibility. Studies showed that stress and anxiety management techniques on rehabilitation or reduction of injury, had a positive effect. More specifically, these management programs have been affective in decreasing negative thinking and increasing performance [14], and increasing pain tolerance [51]. This experience produces a sense of accomplishment and facilitates recovery [54]. Furthermore, physiological changes indicating an improvement in relaxation, such as decreases in heart rate, respiration rate, and blood pressure, have been demonstrated with relaxation technique [30, 41, 57]. Relaxation training is reported to assist an injured athlete to cope with pain and affect the sympathetic nervous system to aid healing [70]
Imagery
Another technique that may be useful to cope with pain is the use of healing images, related to successful physical outcomes. Imagery has been defined by Denis [18] as a psychological activity that “brinks out” the physical characteristics of an object, person, or place that is either permanently or temporarily absent from ones perception. Images can either be passive reproductions or active and dynamic [48]. The athlete could be given a clear description of what has happened internally as a result of the injury and the subsequent process of healing. The therapist may help the athlete to create the visual images that can be utilized in the imagery process [31].
Also, athletes often picture themselves performing the feats of their respective sports. In the event of an injury, sports medicine professionals can encourage injured athletes to tap into this skill and apply it to the various phases of the recovery process (e.g while receiving treatment, to attain rehabilitation goals). Using imagery can return a sense of control to injured athletes: At this stage they cannot physically perform an activity, envisioning a successful performance is the next best thing.[15]
Used as an adjunct to therapy, imagery allows athletes to achieve specific mindsets for maintaining a positive outlook, controlling stress, and sustaining belief in the rehabilitation process [28]. Incorporating imagery into the rehabilitation sessions improves confidence and instils a sense of control over the injured part. Many of the mental exercises can be performed during therapies such as whirlpool; bike riding; ultrasound; and electrical muscle stimulation [28] to better cope with internal and external pain, to expedite the recovery process, and to keep physical skills from deteriorating [55].
Imagery has been the subject of numerous studies for over 80 years, and meta-analyses have been conducted regarding its application [22]. Many sport psychologists and medical practitioners have documented their belief in the potential value of imagery [9, 20, 29, 31, 35, 49] and its ability to speed up the recovery process [29, 32, 55] and even been used as a tool for prevention [17]. In many instances, practitioners have successfully combined a program of relaxation with imagery to enhance recovery following surgery [20]. Research has also demonstrated that greater flow and warmth to the injured area (thereby promoting healing) has been facilitated by imagery [8].
Information about setbacks in performance
At this stage, it is also very crucial to prepare the athletes for potential setbacks and plateaus in the rehabilitation process [15]. Typically, injured athletes view setbacks negatively because they are usually unexpected for them and upsetting. That’s why setbacks usually lead to worry, frustration, depression and anxiety.
The reorientation of athletes about setbacks begins with information. A good place to start is to replace the word “setback” with one that is more accurate and descriptive of what is happening to their body. The reality of setbacks is that they serve a specific and necessary function in the recovery process. In other words, setbacks may be better characterized as an important part of the healing process that gives valuable information about the pace and progress of a current rehabilitation regimen. According to Fisher [24], plateaus are simply periods of necessary neural consolidation and integration, which are necessary before “breakthroughs” can occur. There is a parallel to be drawn between learning a sport skill and rehabilitation progress. Skill, strength, endurance and range of motion gains are realized in smaller and smaller increments at advanced stages. This is the law of diminishing returns. Injured athletes cannot expect the same rate of progress later in their rehabilitation as they achieved earlier. Unless this reality is accepted, athletes are bound to become frustrated with their lack of progress, and this may negatively affect their beliefs and expectations [24].
In other words, what is called “setbacks”, are often necessary periods during which what has been achieved in physical therapy is established. In this perspective, the term that would rather be used instead of setbacks is “healing cycle” [31]. The use of the term “healing cycle” relieves athletes because healing is what they expect. So, these difficult periods are a productive part of rehabilitation. Injured athletes must also understand that their problems are temporary. In summary, when healing cycles appear, patients should be encouraged to recognize their value or cause and take active steps to overcome them.
Restoration of joint stability
Continuing the rehabilitation process and after regaining enough painless range of motion, the therapist introduces more complex motor patterns that contain coordination and balance. At this moment, the specific rehabilitative goal is the restoration of joint stability and motor control of the injured limb [56]. The issue is that the mechanoreceptors found in the tendons, muscles, ligaments and capsule of the joint are usually also injured and it is believed that they lose their proprioceptive ability. In other words, deficits in joint proprioception results in decreased neuromuscular control [56]. These proprioceptive rehabilitation programs usually prescribe balance-training devices, such as unstable balance platforms [40, 56, 66].
For example, after a knee ligament injury, the athlete is asked to stand on a single leg on the platform with both arms on his waist and with the unsupported limb held in a comfortable position so as not to contact the injured limb or the platform [56]. Instructions are usually given to the participants to focus on a visual feedback screen directly in front of them and attempt to maintain the cursor, at the centre of the bullseye on the screen. This is the static balance component of the program.
There is also the dynamic part of the program where the athlete is asked to actively move the platform within a specified range or in a circular direction to “chase” a moving object. The athlete “chases” a moving point on the computer screen by tilting the platform, attempting to keep the balance point near the moving point on the computer screen by relying on visual feedback from the balance device [34].
Imagery
In order to improve the stability performance, the injured athlete needs to understand how the sensorimotor system works. Imagery can facilitate achievement of these rehabilitative skills and outcomes by helping athletes visualize the desired effect of exercises [59]. Imagery strategies include 3 types of rehearsal: visual, emotive imagery and body [46]. Visual may include mastery and coping rehearsal. On mastery, the athlete builds his motivation for rehabilitation and confidence upon the return to competition. On coping, athlete visualises the negative aspects of problematic situations that may occur during the rehabilitation program and learns to overpass them. Emotive rehearsal enables the athlete to feel secure and confident that rehabilitation will be successful. Finally, during body rehearsal the athlete thries to see vividly what happens to the injury internally during the rehabilitation process. Full detailed explanation of the injury, is necessary.
An anatomical model can be used to aid understanding of how these specific rehabilitation exercises will impact on the injured joint. Envisioning the static and dynamic components of the specific joint the athlete creates the mind-set required for optimal performance. Understanding the body’s inner workings and the structural damage caused by the trauma can help athletes gain control over the injury [55].
Describing how the stability system works, it is evident that, both static and dynamic training programs involve balance and a more complex use of muscle groups [1], meaning that athletes have to be able to be concentrated and keep their attention on the exercising leg. Otherwise, patients will not be able to benefit the most by this exercise. This means that, athletes must have two things in mind: First, remain focused on the visual feedback screen and second maintain the position described before.
Relaxation
In order to keep their attention, athletes can apply a simple kind of relaxation technique before the beginning of the training session. It is very important at this point to remember that athletes should perform these exercises in a quiet and isolated room without any distractions. Even if isolated training rooms are not suggested for injured athletes, nevertheless only for stability exercises athletes need to be effectively concentrated.
Self talk
Self talk is an integral dialogue athletes are engaged in, which determines their interpretation of the situation and, in turn, their physical and psychological reaction to it [16].
This internal dialogue may contain either positive or negative thoughts depending on the emotional state of the athlete. During all the rehabilitation period, the therapist is trying to replace the negative thoughts with positive ones in order to motivate the athlete to work through rehabilitation with confidence and sustained effort.
At this stage, the athlete should be encouraged to use the instructive self-talk which serves to enhance the athlete’s effort and help him stay focused at the stability exercise and maintain the right body position described above. This technique is very useful at this moment because it is imperative that the athlete keeps the right joint angle in order to be able to benefit the most by this exercise. An example of an instructive phrase that can be used is “focus on the knee”. It is better to encourage your athletes to repeat this phrase loud and clear [6].
Muscular strengthening
As joint motion and flexibility return, resistance exercises are introduced in order to avoid important losses of strength, power and endurance. The purpose of progressive resistance exercise in sport and in therapy is to increase muscle strength and size, and to decrease the risk of re-injury [68]. Usually strengthening programs start with limited-range isotonic exercises, and then achieve excellent and rapid results with isokinetic machine.
Goal-setting
Collaborative goals should be set at each exercise session to help both the injured athlete and the therapist to focus on each step of the rehabilitation process [26]. Short-term (e.g weekly) medium term (e.g monthly) and long term (e.g 6-12 months) goals will also need to be established depending on the severity of injury and possibly the duration of the rehabilitation. For example, “today I have executed 3sets of 15 repetitions with 10kgr weights. Tomorrow I will accomplish 4 sets or 20 repetitions”. When athletes are ready to accomplish more sets and more repetitions with the same weight, then they can set goals to increase the weight.
Goal setting is also proved to maximize the isokinetic performance of injured athletes [64, 65]. It is well known that isokinetic exercises use equipment in which the speed of movement is pre-set and the resistance athletes get is adapted to match the force they apply [2]. This basic characteristic means that, the more athletes try the more resistance they receive from the machine. When they get tired, they reduce their effort, and the resistance is also reduced. That is really a very important advantage for injured athletes, because they train safely and maximally at the same time.
But, in order to obtain the maximum results, athletes have to give the maximum of their effort during all the range of motion and all the repetitions. It has been shown that goal setting can be very helpful for injured athletes to overcome their fatigue and increase their effort [44]. Particularly, it has been shown that injured athletes who set goals for each of their isokinetic strength training sessions improved their performance a lot more than injured athletes who trained without setting goals [5, 6, 64, 65]. In specific, the goal setting group proved to increase both self efficacy and performance self satisfaction and decrease anxiety indicating also change of athletes’ behaviour because of the technique applied. The authors concluded that the injured athletes who used goal setting behaved in a similar manner to no injured athletes, indicating that this technique may be appropriate to increase their effort and build their confidence [64, 65].
Positive Self-talk
Positive self-talk serves to motivate the athlete to work through rehabilitation with confidence and sustained effort [15]. Positive self-statements such as “I’m getting stronger everyday” should be read several times a day or when athletes feel they need a reminder to think positively. Bunker, Williams and Zinsser [11], indicated that self talk is one of the major secrets to control the mind. Positive self talk helps and directs the athletes to keep their minds in the present (in what they are doing right now). Also, helps them stop calling off their minds from negative thinking and past mistakes, and not to worry of what might happen in the future.The effectiveness of self-talk is proved to facilitate the isokinetic performance by focusing and directing the attention (concentrating) of the participant [62]. Athletes who saw positive self-statements at a computer screen in front of them while they were exercising in the isokinetic machine. “I feel good” “I am getting strong” etc [62]. In another research, athletes set goals for each performance, then they chose their favourite statement and they executed the exercise having their goal in mind and looking at their statement on the screen. That group improved their strength faster than the control group and appeared plateaus of smaller duration [5].
Sport-related skill training
As a last component of rehabilitation, specific skill patterns and sport-related skills are prescribed, with progressively complex drills meaning that the use of the injured area becomes more realistic and comparisons to how it “used to work” become more usual. Unfortunately, these comparisons are not favourable because performance is initially dramatically below pre injury levels [6]. These pessimistic evaluations can lead to frustration and focus on negative aspects of the injury. Furthermore at this last step, athletes usually have the fear of re-injury, resulting in decreased effort.
Direct their attention
To address the comparisons with previous performance, it is really important to provide the athletes with information and skills to maintain a positive focus and ensure maximum benefit. Give them the message that their progress is gradual and they have to be patient like when they learn a new skill. Direct their attention to everything they have accomplished from the beginning of the rehabilitation period.
Goal setting and self talk
During these later stages of recovery, appropriate goal setting is still essential when motivation or fear of re-injury are possible problems, particularly in long-term rehabilitation [19, 21, 52]. It can provide motivation and commitment, direct the athlete’s attention to controllable factors and help them build confidence, since they may be afraid that they αre not ready to return to their sport. They may also be concerned about their form or status within the team [31]. Therapists can assist by encouraging athletes to develop positive self-talk and to think about success in rehabilitation, to manage setbacks and ultimately, to return to their sport successfully [26]. It is also vital that we educate our athletes against their reaction of returning to the team earlier and to ensure that they have full recovered and are back to their pre-injury level of athletic performance.
Bibliography and the additional learning materials
Apparently, if athletic trainers and physical therapists, want to be successful they must be able to interact with injured athletes effectively. Applying simple techniques as those mentioned in the present article throughout the rehabilitation period, athletes can be motivated and prepared to deal with the injury’s barriers.Cognitive Therapy and Research 1991; 15: 1-19.
1. Ashton-Miller J, Wojtys E, Huston L, Fry-Welch D. Can proprioception really be improved by exercise? Knee Surgery and Sports Traumatology, Artroscopy 2001; 9: 128-136.
2. Baltzopoulos V, Brodie DA. Isokinetic dynamometry: Applications and limitations. Sport Medicine 1989; 8: 101-116.
3. Bassett SF, Petrie KJ. The effect of treatment goals on patients compliance with physiotherapy exercise program. Physiotherapy 1999; 85: 130-137.
4. Beneka A, Malliou P, Theodorakis Y, Antoniou P, Godolias G. The application of positive self-talk in muscular performance. In World Sport Science Congress, Adelphi University, New York 1998; p. 103.
5. Beneka A, Malliou P, Theodorakis Y, Godolias G, The effect of self talk and goal setting in muscular performance on knee injured athletes during the rehabilitation period. Science-Security-Police, Journal of Police Academy, 2000, 1: 105-122.
6. Beneka Α. Implementing mental skills training technique in the physical rehabilitation plan of the injured athlete. In VIIth IOC Olympic World Congress on Sport Sciences, Athens 2003. p. 21A.
7. Bianco T, Malo S, Orlick T. Sport injury and illmess: Elite skiers describe their experiences. Research Quarterly for Exercise and Sport 1999; 70: 157-169.
8. Blakeslee TR. The right brain. New York: Anchor Press; 1980.
9. Brewer BW, Jeffers KE, Petitpas AJ, Van Raalte JL. Perceptions of psychological interventions in the context of sport injury rehabilitation. The Sport Psychologist 1994; 8: 176-188.
10. Brewer BW. Review and critique of models of psychological adjustment to athletic injury. Journal of Applied Sport Psychology 1994; 6: 87-100.
11. Bunker, L., Williams, J.M., & Zinsser, N. 1998. Cognitive techniques for improving performance and building confidence. In J.M. Williams (Ed.) Applied sport psychology (2nd ed., pp.225-242). Palo Alto, CA: Mayfield.
12. Carroll S. Mental imagery as an aid to healing the injured athlete. In Annual meeting of the Association for the Advancement of Applied Sport Psychology, Lake Tahoe, NV, October 1994.
13. Chung Y, Gould D. Identifying barriers to psychological skills training in the training room: A survey of athletic trainers. In 10th World Congress of Sport Psychology, Skiathos 2001. p. 112-114.
14. Crocker, P.R.E., Alderman, R.B., & Smith, F.M.R. Cognitive-affective stress management training with high performance youth volleyball players: Effects on affect, cognition, and performance. Journal of Sport and Exercise Psychology 1988; 10, 448-460.
15. Crossman J. Coping with Sports Injuries: Psychological strategies for rehabilitation. New York: Oxford University Press; 2001.
16. Crossman J. Managing thought, stress and pain. In Crossman J. Coping with Sports Injuries: Psychological strategies for rehabilitation. New York: Oxford University Press; 2001. p. 128-147.
17. Davis JO. Sport injuries and stress management: An opportunity for research. The Sport Psychologist 1991; 5: 175-182.
18. Denis, M. Visual imagery and the use of mental pracitce in the development of motor skills. Canadian Journal of Applied Sport Sciences 1985; 10: 4S-16S.
19. DePalma MT, DePalma B. The use of instruction and the behavioral approach to facilitate injury rehabilitation. Journal of Athletic Training 1989; 24: 217-219.
20. Durso-Cupal DD. The efficacy of guided imagery for recovery from anterior cruciate ligament (ACL) replacement. Journal of Applied Sport Psychology 1996; 8 Suppl: 56.
21. Ermler KL, Thomas CE. Interventions for the alienating effect of injury. Journal of Athletic Training 1990; 25: 269-271..
22. Feltz DL, Landers DM. The effects of mental practice on motor skill learning and performance: A meta-analysis. Journal of Sport Psychology 1983; 5: 25-27.
23. Fisher AC, Mullins SA, Frye PA. Athletic trainers’ attitudes and judgements of injured athletes’ rehabilitation adherence. Journal of Athletic Training 1993; 28: 43-47.
24. Fisher AC. Counseling for Improved Rehabilitation Adherence. In Ray R, Wiese-Bjornstal DM (Eds). Counseling in Sports Medicine. Champaign IL: Human Kinetics; 1999. p. 275-292.
25. Ford IW, Gordon S. Perspectives on the psychological curricula in professional training programs of sport physiotherapists and sport/athletic trainers: a cross-cultural survey. In Annual meeting of the Association for the Advancement of Applied Sport Psychology, Lake Tahoe, NV, 1994.
26. Gordon G, Potter M, Hamer P. The role of the physiotherapist and sport therapist. InCrossman J. Coping with Sports Injuries: Psychological strategies for rehabilitation. New York: Oxford University Press; 2001. p. 62-82.
27. Gordon S, Lidgren S. Psycho-physical rehabilitation from a serious sport injury: Case study of an elite fast bowler. Australian Journal of Science and Medicine in Sport 1990; 22: 71-76.
28. Granito V, Hogan J, Varnum L. The performance Enhancement Group Program: Integrating sport psychology and rehabilitation. Journal of Athletic Training 1995; 30(4): 328-331.
29. Green LB. The use of imagery in the rehabilitation of injured athletes. The sportPsychologist 1992; 6: 416-428.
30. Hardy L. Psychological stress, performance and injury in sport. British Medical Bulletin 1992; 48: 615-629.
31. Heil J. Psychology of sport injury. Champaign IL: Human Kinetics; 1993.
32. Ievleva L, Orlick T. Mental links to enhanced healing: An explanatory study. The Sport Psychologist 1991; 5: 25-40.
33. Johnston LH, Carroll D. The context of emotional responses to athletic injury: A qualitative analysis. Journal of Sport Rehabilitation 1998; 7: 206-220.
34. Johnston RB, Ηoward ME, Cawley PW, Losse GM. Effect of lower extremity muscular fatigue on motor control performance. Medicine & Science in Sports & Exercise 1998; 30(12): 1703-1707.
35. Jones L, Stuth G. The uses of mental imagery in athletics: An overview. Applied and Preventive Psychology 1997; 6: 101-115.
36. Kolt G. Psychological services in sport injury rehabilitation: The role of nonpsychologist rehabilitation personnel. In 10th World Congress of Sport Psychology, Skiathos, 2001. p. 110-113.
37. Lamott EE, PetlichkoffLM. Psychological factors and the injured athlete: Is there a relationship? In the Annual meeting of the Association for the Advancement of Applied Sport Psychology, San Antonio, TX, September 1990.
38. Lamott EE, PetlichkoffLM. Van Wassenhove J, Stein K, Wade G, Lewis K. Psychological rehabilitation of the injured athlete: An educational approach to injury. In the Annual meeting of the Association for the Advancement of Applied Sport Psychology, Seattle, WA, 1989.
39. Larson GA, Starkey C, Zaichkowsky LD. Psychological aspects of athletic injuries as perceived by athletic trainers. The Sport Psychologist 1996; 10: 37-47.
40. Lentell GL, Katzman LL, Walters MR. The relationship between muscle function and ankle stability. J Orthop Sports Phys Ther 1990; 11: 605-611.
41. Lichstein KL. Clinical relaxationstrategies. Wiley, New York; 1988.
42. Locke, E.A., Shaw, K.N., Saari, L.M., &Lathram, G.P. Goal setting and task performance. Psychological Bulletin 1981; 90: 125-152.
43. MacWhannell DE. Communication in physiotherapy practice. In French S. Physiotherapy: A psychological approach. Oxford, England: Butterworth-Heinemann; 1992. p. 98-112.
44. Malliou P, Beneka A, Aggelousis N, Theodorakis Y. Goal setting: An efficient way to maximise isokinetic performance. Isokinetic and Exercise Science 1998; 7: 11-17.
45. Meichenbaum D, Turk DC. Facilitating treatment adherence. New York: Plenum 1987.
46. Moss, R.H. The crisis of illness: An overview in coping with physical illness. New York: Plenum Medical Book Co.
47. Nathan B. Touch and emotion in manual therapy. London: Churchill Livingstone; 1999.
48. Paivio, A. Mental representations. New York: Oxford University Press.
49. Pargman D. Psychological bases of sport injuries. Fitness Information Technology, Morgantown, West Virginia; 1993.
50. Pen LJ, Fisher AC, Sforzo GA, McManis BG. Cognitive strategies and pain tolerance in subjects with muscle soreness. Journal of Sport Rehabilitation 1995; 4: 181-194.
51. Pen LJ, Fisher AC. Athletes and pain tolerance. Sports Medicine 1994; 18: 319-329.
52. Porter K, Foster J. Who will stop the pain? Overcome your injuries with a program of positive imagery. World Tennis 1987; 35: 28-30.
53. Potter M, Grove JR. Mental skills training during rehabilitation: Case studies of injured athletes. New Zealand Journal of Physiotherapy 1999; 28: 24-31.
54. Ray R, Wiese-Bjornstal DM. Counseling in Sports Medicine. Champaign IL: Human Kinetics; 1999.
55. Richardson PA, Latuda LM. Therapeutic imagery and athletic injuries. Journal of Athletic Training 1995; 30: 10-12.
56. Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for person with functionally unstable ankles. Journal of Orthopaedic& Sports Physical Therapy 1999; 29(8): 478-486.
57. Singer RN, Johnson PJ. Strategies to cope with pain associated with sport-related injuries. Journal of Athletic Training 1987; 22: 100-103.
58. Smith AM, Milliner EK. Injured athletes and the risk of suicide. Journal of Athletic Training 1994; 29: 337-341.
59. Sordoni C, Hall C, Forwll L. The use of imagery by athletes during injury rehabilitation. J Sport Rehabil. 2000; 9: 329-338.
60. Sparkes AC. An Achilles heel to the survival of self. Qualitative Health Research 1998; 8: 644-664.
61. Taylor J, Taylor S. Psychological approaches to sports injury Rehabilitation, Gaithersburg, Maryland: Aspen Publishers Inc; 1997.
62. Theodorakis Y, Beneka A, Goudas M, Antoniou P, Malliou P. The effect of self-talk on injury rehabilitation. European Yearbook of sport psychology 1998; 2: 124-135.
63. Theodorakis Y, Beneka A, Goudas M, Antoniou P, Malliou P. The effect of self-talk on injury rehabilitation. Journal of Applied Sport Psychology 1997, 12(2 Suppl): S164.
64. Theodorakis Y, Beneka A, Malliou P, Goudas M. Examining psychological factors during injury rehabilitation. Journal of Sports Rehabilitation 1997; 10: 372-381.
65. Theodorakis Y, Malliou P, Papaioannou A, Beneka A, Filaktakidou A. The effect of Personal Goals, Self Efficacy and Self Satisfaction on Injury Rehabilitation. Journal of Sport Rehabilitation 1996; 5: 214-223.
66. Tropp H. Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985; 6: 180-182.
67. Udry E, Gould D, Bridges D, Beck L. Down but not out: Athlete responses to season-ending injuries. Journal of Sport and Exercise Psychology 1997; 19:229-248.
68. Wajswelner H, Webb G. Therapeutic exercise. In Zuluaga M, Briggs C, Carlisle J, McDonald V, McMeeken J, Nickson W, et al. Sports Physiotherapy. Applied science and practice. Melbourne: Churchill Livingstone; 2000. p. 207-221.
69. Wiese DM, Weiss MR, Yukelson D. Sport psychology in the training room: A survey of athletic trainers. The sportPsychologist 1991; 5: 15-24.
70. Wiese DM, Weiss MR. Psychological rehabilitation and physical injury: Implications for the sports medicine team. The Sport Psychologist 1987; 1: 318-330.
71. Williams SL, Kinney PJ. Performance and nonperformance strategies for coping with acute pain: The role of perceived self-efficacy, expected outcomes, and attention. Cognitive Therapy and Research 1991; 15: 1-19.
[ays_quiz id=’18’]
Erasmus+
“This project has been funded with support from the European Commission. This publication reflects the views only of the author, and the Commission cannot be held responsible for any use which may be made of the information contained therein.”